Caring for Hospitalized Patients with Diabetes, Hyperglycemia and COVID-19: Bridging the Remaining Knowledge Gaps
Feb 9, 2021, 11:06 AM
By Grace Prince, MD; Amisha Wallia, MD, MS; Jane Jeffrie Seley, DNP, MPH, CDCES, BC-ADM
The COVID-19 pandemic (caused by SARS-CoV-2) has devastated countries across the globe. A history of diabetes as well as significant hyperglycemia have been associated with higher risk of severe disease from SARS-CoV-2. This is not surprising given the association between infection/inflammation and hyperglycemia. Individuals across the globe with COVID-19 have presented with concurrent hyperglycemic crises; some have required extremely high doses of insulin due to pronounced insulin resistance. During the pandemic, frequent glucose monitoring and dosing of insulin became challenging due to increased face-to-face time with COVID-positive patients. As cases climbed, attention to the interplay between diabetes/hyperglycemia and patient outcomes, as well as novel therapeutic approaches, quickly became a priority.
COVID-19, Diabetes and Hyperglycemia
A retrospective study of 88 hospitals in the United States examined 1122 patients with SARS-CoV-2 infection. A significantly higher mortality rate (28.8%) was seen in patients with diabetes. Among patients without diabetes who had hyperglycemia (> 2 blood glucoses > 180 mg/dL in 24 hours), mortality was increased compared to those without hyperglycemia (6.2%, p<0.001). The sub-group with significant hyperglycemia had a higher mortality (40/96) compared to those with diabetes alone (13/88, p<0.001) [DOI: 10.1177/1932296820924469]. Increased morbidity in patients with diabetes/hyperglycemia (increased rates of acute respiratory distress syndrome, acute heart and kidney injury, septic shock and disseminated intravascular coagulation), have been seen in other studies.
Therapeutic Approach
Though the link between significant hyperglycemia and poorer outcomes was identified fairly early in the pandemic, managing hyperglycemia posed numerous challenges. In addition to hyperglycemia resulting from acute inflammation and infection, patients who are critically ill with COVID-19 require therapeutics (e.g. steroids, vasopressors, supplemental nutrition) that exacerbate insulin resistance.
Insulin has long been the mainstay of inpatient diabetes therapy and likely represents the best therapeutic option for patients with COVID-19. Notably, insulin administration is challenging during a surge, particularly for critically ill patients on insulin infusions, which require frequent monitoring to modulate rates. Nevertheless, with its short half-life and ability to be quickly titrated, insulin infusions and frequent blood glucose monitoring are still preferred, especially as sudden resolution of severe insulin resistance has been observed.
Changing Protocols & Emerging Technologies
Care delivery during the pandemic was rapidly streamlined to minimize healthcare worker (HCW) exposures. Nurses “bundled” care when entering a patient room, for example, limiting the frequency and coordinating the timing of glucose checks with other interventions, particularly insulin administration or insulin infusion titration. On a site-by-site basis, inpatient diabetic ketoacidosis (DKA) protocols were modified based on existing literature to include dosing of rapid-acting subcutaneous insulin every four hours as an alternative to intravenous insulin for treatment of mild-to-moderate DKA.
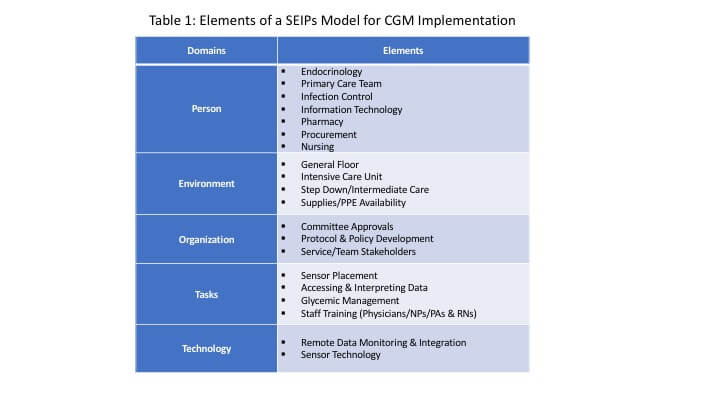
The Food and Drug Administration exercised “enforcement discretion” for temporary, off label hospital use of continuous glucose monitoring (CGM) during the pandemic. Pre-COVID-19, randomized controlled trial data demonstrated that CGM use reduces inpatient hypoglycemia in patients with type 2 diabetes on insulin [DOI: 10.2337/dc20-0840], and is associated with a significantly lower mean glucose and increased time in range for patients in the non-intensive care units [DOI: 10.2337/dc20-1016]. Given accuracy concerns in critically ill patients, CGM may be most appropriate for non-critically ill patients. As institutions evaluate the benefits and feasibility of remote monitoring with CGM, frameworks like the quality implementation framework and systems engineering model for patient safety (SEIPs) can help with planning and implementation (Table 1).
Overall, as cases of COVID-19 surged and risk factors for more severe disease became apparent, existing inpatient diabetes care, which required frequent glucose monitoring, insulin administration and face-to-face time, had to be critically evaluated and adapted. Decisions shaping patient care delivery were informed by a combination of pre-pandemic, evidence-based practice, rapidly emerging data, and first-hand experience. Through a time of crisis, there was focused collaboration between institutions and communities to bend the curve on COVID-19 and diabetes. Frameworks were modified to safely meet patient needs while protecting HCWs. As the pandemic evolves, it remains imperative that we continue to share data and information rapidly and judiciously.
Click here to access Caring for Hospitalized Patients with Diabetes, Hyperglycemia and COVID-19: Bridging the Remaining Knowledge Gaps.
ADCES Perspectives on Diabetes Care
The Association of Diabetes Care & Education Specialists Perspectives on Diabetes Care covers diabetes, prediabetes and other cardiometabolic conditions. Not all views expressed reflect the official position of the Association of Diabetes Care & Education Specialists.
Copyright is owned or held by the Association of Diabetes Care & Education Specialists and all rights are reserved. Permission is granted, at no cost and without need for further request, to link to, quote, excerpt or reprint from these stories in any medium as long as no text is altered, and proper attribution is made to the Association of Diabetes Care & Education Specialists.
HEALTHCARE DISCLAIMER: This site and its services do not constitute the practice of medical advice, diagnosis or treatment. Always talk to your diabetes care and education specialist or healthcare provider for diagnosis and treatment, including your specific medical needs. If you have or suspect that you have a medical problem or condition, please contact a qualified health care professional immediately. To find a diabetes care and education specialist near you, visit DiabetesEducator.org/Find.