Expanding diabetes technology access and enabling data-informed care for a broader population
With the introduction of connected insulin pens and caps, the most common insulin delivery method globally (1) has entered the digital age. This has expanded diabetes technology access and enabled data-informed care for a broader population. The data from these devices are shining the spotlight on multiple daily insulin injection therapy, revealing opportunities to significantly improve care for this population (2). "Tracking" insulin pens or caps keep track of insulin doses delivered by the device, while "smart" insulin pens track doses including active insulin and provide dose recommendations based on current glucose levels, active insulin, and programmed insulin therapy settings (3).
Clinical challenges of insulin injection therapy: Delivering the right dose at the right time
Connected insulin injection technologies help address clinical challenges with insulin injection therapy including (3):
- Accurate delivery of the intended insulin dose (precision dosing)
- Delivering the right dose at the right time (reducing missed, mistimed, and mismatched insulin doses)
- Providing data to the care team to help inform timely therapy decisions
Accurate delivery of the intended dose (precision dosing)
Individuals prescribed insulin injection therapy must be trained on appropriate insulin injection technique and rotation of insulin injection sites, the importance of priming before each rapid acting insulin dose and assuring the integrity of the insulin being injected. An annual check of insulin injection technique and physical palpation of insulin injection sites is recommended (or more often if there is unexplained hyperglycemia) (4). A smart insulin pen can distinguish between prime and therapy doses to accurately track active insulin on board from previous doses, necessary for safe and effective dose recommendations (2). Temperature and age sensors, available with some connected insulin pens, alert users if the insulin integrity is at risk.
How do you deliver the right dose at the right time (reducing missed, mistimed, and mismatched insulin doses)?
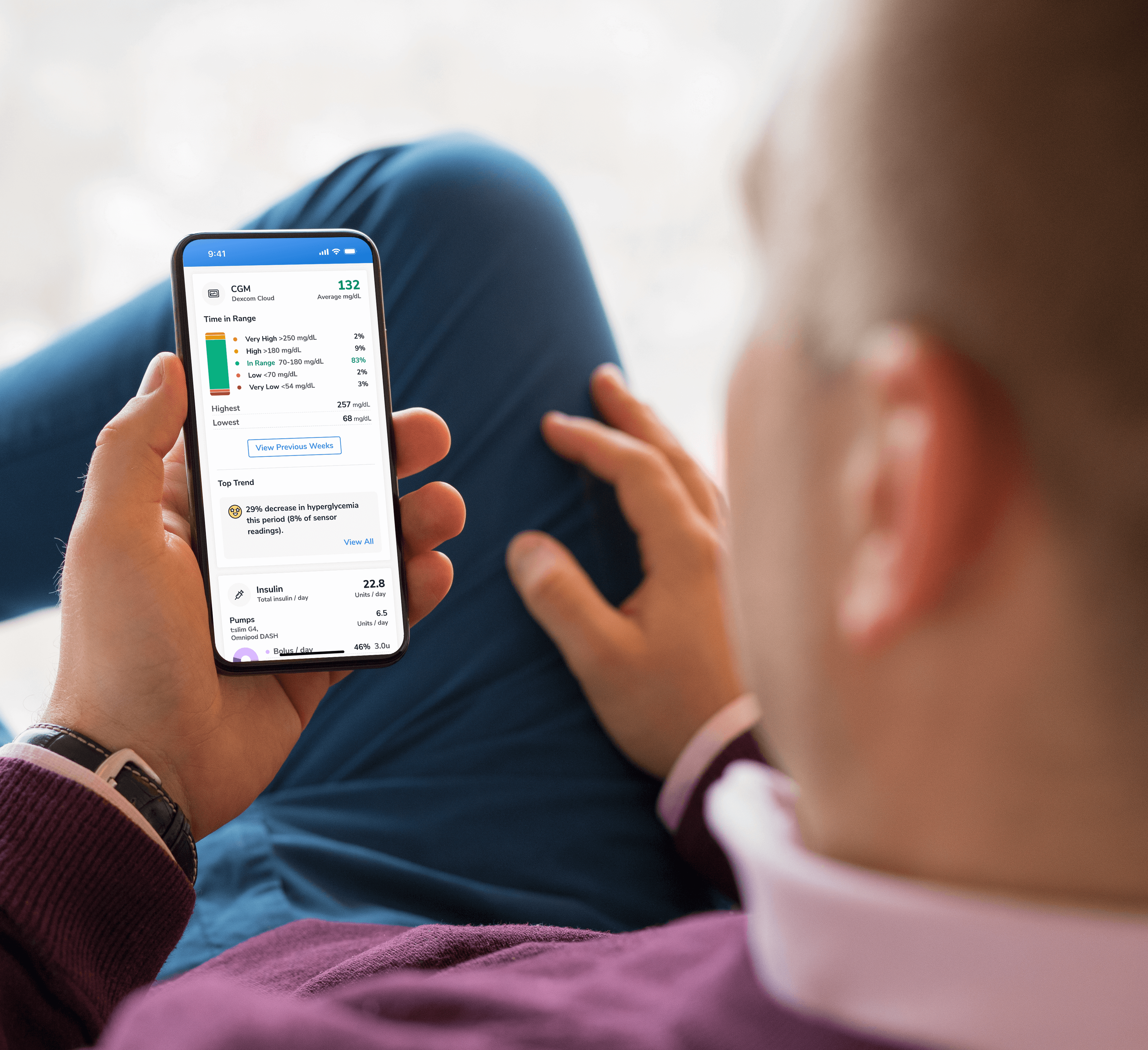
Individuals on injection therapy need support in determining the right dose to take at the right time. Missed, mistimed, and mismatched insulin bolus doses occur commonly in all ages, in people with type 1 or type 2 diabetes and are associated with higher A1C (2). Individuals report that disruptions in their daily routine, social or work situations and concerns about hypoglycemia contribute to mistiming of their insulin doses (5). To help avoid forgetting to dose, smart insulin pens can provide missed dose alerts when users do not dose during a pre-defined mealtime period. If individuals cannot remember if they dosed or not for food they ate, they can check their smart insulin pen app to find when they last dosed, how much was dosed, and the amount of active insulin on board from previous doses, to avoid repeating or missing doses. By combining dosing data with CGM data it is possible to provide glucose alerts only when action is needed and not when a correction dose would not be safe based on active insulin, thus helping to reduce alarm fatigue. It is projected that future smart insulin pens will use meal detection technology to alert users to dose their insulin if a dose were omitted and artificial intelligence will determine and fine-tune insulin therapy settings and titrate insulin doses.
Limited numeracy skills in a number-rich condition such as diabetes contributes to insulin management challenges. Research in people with diabetes on insulin therapy reports that over half were unable to calculate an insulin dose when provided a glucose level and specific amount of carbohydrate (6). Smart insulin pens provide dose recommendations for food and correction doses, accounting for active insulin from previous doses, and based on individualized insulin therapy settings including insulin-to-carbohydrate ratio and insulin sensitivity factor (7). Smart insulin pen dose calculators can also provide simpler fixed-dose insulin plans for individuals adjusting their dose based on their relative meal size (small, medium, large).
Providing data to the care team to help inform timely therapy decisions
There are many barriers to timely insulin titration and ongoing insulin management in clinical practice including lack of time, resources, expertise or experience to design insulin therapy plans, make frequent dose adjustments, and provide education (8). The American Diabetes Association (ADA) recommends adjusting insulin doses every few days until glycemic goals are met with ongoing adjustments as insulin requirements change over time (9). Having data available can inform more timely therapy adjustments and shifts the insulin therapy discussion to be less interrogative and more collaborative (10). An expert panel has published recommendations for a standardized ambulatory glucose profile report for connected insulin pens integrated with CGM data with the goal of simplifying insulin management (11). Automated dose, glucose, and meal data recording and sharing are replacing the traditional inaccurate and incomplete logbook giving the clinical team a more comprehensive picture of insulin therapy, self-management practices, and the impact on glycemia (12, 13).
Clinical practice guidelines
The ADA discusses the importance of individual preference considering cost, insulin plan, and self-management ability when choosing a method of insulin delivery and advises that clinician input and education are useful for determining the initial insulin therapy settings and for ongoing adjustments. The ADA recommends that connected insulin pens with their capacity to record and transmit data may be used for those on injection therapy and that FDA-approved insulin dose calculators/decision support systems may be helpful for calculating insulin doses (9).
What is the role of the diabetes care and education specialist in precision insulin injection management with connected insulin pens?
The diabetes care and education specialist (DCES) is critical in supporting individuals on insulin therapy including when introducing new technologies and when there are transitions in insulin therapy (14). The Association of Diabetes Care & Education Specialists Identify-Configure-Collaborate (ICC) framework is a standardized approach for technology integration into clinical practice (15) to help improve technology access and enable data-informed care (16). This approach is critical to precision insulin management (supporting individuals in delivering the right dose at the right time plus timely insulin plan adjustments) for injection therapy (3).
Identify. The DCES leads in making sure that every individual on insulin therapy is assisted in making informed choices regarding their preferred method of insulin delivery considering cost, perceived complexity, and convenience (17).
Configure. The DCES leads in assuring connected insulin injection technologies are configured for the personal therapy plan and preferences of the individual including (3):
1) Calculate and program individualized insulin therapy settings.
2) Adjust the meal schedule in the app to match the individuals’ usual routine; turn on desired missed dose alerts and glucose check reminders; connect to available Bluetooth-enabled glucose monitoring devices.
3) Agree on a plan for sharing the data with the care team.
4) Provide current prescriptions for insulin and/or cartridges and related supplies and connected glucose monitoring supplies; address any cost concerns.
5) Teach/check insulin injection technique, discussing the importance of priming, injection site rotation, and proper insulin storage.
6) Together select one or two priorities from the list below to help integrate the technology into the individual’s self-management routine:
- Unsure if dosed: Advise to check the app home screen for the last dose amount and time, last glucose and any active insulin.
- Forgets to dose: Set missed dose alerts for usual mealtimes.
- Unsure how much to dose for meals and corrections: Advise to check glucose and use the bolus calculator when dosing.
- While fine-tuning settings and learning carbohydrate counting, ask if the individual would be willing to check their glucose two hours after their mealtime doses to see if a correction dose is needed.
- Keeping records of diabetes data: Encourage individuals to log additional insulin doses if taken without the connected insulin injection technology; suggest regular review of the app log as needed for daily history and adjust reminders for doses and glucose checks as needed.
- Upcoming care team touchpoint: Encourage individuals to share data reports and engage with the care team at and between health care visits per plan.
- The care plan has been adjusted: Update Insulin Therapy Settings as the care plan evolves.
Collaborate. The collaborative use of the resulting data with the care team to assess and address barriers to following the agreed upon care plan and to adjust the care plan on a timely basis is critical to adoption of technology and ongoing engagement. Having dose data, integrated with glucose and meal data facilitates precision insulin management (3). A reference guide for building a data-informed practice approach for multiple daily insulin injection therapy with smart insulin pens includes a method for systematic review of smart insulin pen data and is summarized in Table 1 (18).
Table 1. Steps to systematically review smart insulin pen reports (adapted from Warshaw et al, 2020)18
| 1. Review glucose data | - Note average glucose, glycemic variability (standard deviation or coefficient of variation), percent times in-range, below-range, and above-range.
- Check the modal day glucose graph to look for patterns of hypoglycemia, hyperglycemia and/or variability at particular times of day.
- Prioritize resolving hypoglycemia first for safety.
- Note times of day when glucose is within goal and discuss strategies for extending this to other times of day.
|
| 2. Review dose date | - Assess if any insulin doses are regularly missed (mealtime or basal)
- Discuss if missed doses are forgotten, intentionally omitted, or meals are skipped.
- Identify and resolve barriers to taking insulin.
- Adjust meal-time settings and reminders in the app as needed.
- Observe the total daily dose and the distribution between basal and bolus doses.
- Assess the need to optimize the basal insulin dose, with the goal of maintaining glycemic stability in the fasted state with no more than 30 – 50 mg/dL delta.
- Note the average number of boluses per day and consider how this corresponds with the individuals’ reported usual eating pattern.
- Determine if the individual is using the dose calculator at meals and for corrections, and if so, notice if the dose recommendations are followed. If not, explore the root cause considering lack of confidence in their therapy settings or fear of hypoglycemia.
- Assess the glycemic response to mealtime doses and evaluate the adequacy of meal doses or insulin settings.
|
| 3. Review daily charts | - Is glucose checked before each dose?
- Is the meal size or grams of carbohydrate consumed recorded with meal doses? Does the individual need carbohydrate counting/awareness education?
- Would the individual benefit from access to a food database or meal tracking app for help in food recording?
- How many meals does the individual eat per day? Are there any missed meals? If yes, explore why.
- Note the timing of the dose relative to the meal and evaluate if the timing of the insulin dose relative to the meal need adjusting.
- Evaluate glycemic response when the dose calculator is used and the dose recommendation followed versus dosing more or less than recommended. If the dosing recommendations are not followed, explore why.
- Note how often correction doses are taken and determine if there are any missed correction opportunities or any times insulin doses are stacked increasing risk for hypoglycemia.
|
| 4. Adjust therapy settings | - Based on observations and discussions determine if therapy settings or preset mealtime periods need to be adjusted for any time of day or meal in the app in order to avoid falsely triggering missed doses.
|
| 5. Don't forget the basics | - If missing doses, identify and address barriers to taking insulin first prior to adjusting the insulin plan.
- Assure quality of insulin, proper site rotation, injection technique, timing of doses.
- Aways address hypoglycemia first.
- Optimize the basal dose to create a strong foundation for fine-tuning insulin therapy settings to optimize mealtime insulin.
- Fine-tune the insulin-to-carbohydrate ratio or mealtime doses; having mealtime doses correct decreases the need for correction doses.
- Fine-tune the insulin sensitivity factor (correction factor) along with the duration of insulin action and glucose goals as needed.
|
What practice protocols are needed for precision insulin injection management?
The article “Shining the spotlight on multiple daily insulin therapy: real-world evidence of the InPen smart insulin pen” list several person-centered practice protocols needed for data-informed precision insulin management (3).
- Establish roles and responsibilities regarding ongoing technology discussions to be sure every person with diabetes on insulin therapy is helped to make informed decisions regarding their preferred method of insulin delivery.
- Teach and verify appropriate insulin injection technique, site rotation, timing of insulin dose relative to eating, priming, safe insulin storage and rotation of supplies
- Physically palpate insulin injection sites and check on insulin injection technique annually (or more often if unexplained hyperglycemia)
- Optimize the basal insulin dose and identify when to add prandial coverage in type 2 diabetes
- Calculate rapid-acting insulin therapy settings including target glucose, duration of insulin action (active insulin time), insulin-to-carbohydrate ratios or meal doses and insulin sensitivity factor (correction factor) to match individual needs.
- Determine roles and responsibilities for data review including refining the insulin therapy settings and overall care plan on an ongoing basis.
- Develop procedures for virtual care and remote monitoring.
- Prescribe and train on the use of continuous glucose monitoring for individuals on insulin therapy as per current standard of care (8). If using blood glucose monitoring, recommend an optimal blood glucose monitoring schedule to support the prescribed insulin plan.
Data-informed precision insulin injection management is possible with the availability of connected insulin injection technologies. DCESs are encouraged to integrate these technologies in their practice and to develop person-centered practice protocols to address the unmet needs for those in their population on insulin injection therapy. This will expand diabetes technology access and enable data-informed care for all individuals on insulin therapy regardless of how they choose to deliver their insulin.
References:
- Kesavadev J, Saboo B, Krishna MB, Krishnan G. Evolution of insulin delivery devices: from syringes, pens and pumps to DIY artificial pancreas. Diabetes Therapy 2020;11:1251-1269.
- MacLeod J, Im GH, Smith M, Vigersky RA. Shining the spotlight on multiple daily insulin therapy: real-world evidence of the InPen smart insulin pen. Diabetes Technol Thera 2024;26(1):33-39.
- MacLeod J, Vigersky BA. A review of precision insulin management with smart insulin pens: opening up the digital door to people on insulin injection therapy. J Diabets Sci Technol 2023;17:283-289.
- Klonoff DC, Berard L, Denise Reis Franco DR, et al. Advance Insulin Injection Technique and Education With FITTER Forward Expert Recommendations. Mayo Clinic Proceedings 2025;100(4):682-699.
- Robinson S, Newson RS, Liao B, et al. Missed and mistimes insulin doses in people with diabetes: a systematic literature review. Diabetes Technol Ther 2021;23(12):844-856. DOI: 10.1089/dia.2021.0164.
- Zaugg SD, Dogbey G, Collins K, et al. Diabetes numeracy and blood glucose control: association with type of diabetes and source of care. Clin Diabetes 2014;32(4):152-257.
- Harbison R, Hecht M, MacLeod J. Building a data-driven multiple daily insulin therapy model using smart insulin pens. J Diabetes Sci Technol 2022;16:610-616.
- Gabbay RA, Kendall D, Beebe C, Cuddeback J. et al. Addressing therapeutic inertia in 2020 and beyond: a 3-year initiative of the American Diabetes Association. Clinical Diabetes 2020;38(4):371-381.
- American Diabetes Association, Diabetes Technology: Standards of Care in Diabetes—2025. Diabetes Care. 2025;48(Suppl1): S146-S166.
- Kompala T, Neinstein AB. Smart insulin pens: Advancing digital transformation and a connected diabetes care ecosystem. J Diabetes Sci Technol 2022;16:596-604.
- Simonson GD, Criego A, Battelino, et al. Expert panel recommendations for a standardized ambulatory glucose profile report for connected insulin pens. J Diabetes Technology & Therapeutics. 2024; 10.1089/dia.2024.0107 https://www.liebertpub.com/doi/abs/10.1089/dia.2024.0107
- Klonoff DC, Zhang JY, Shang T, Mehta C, Kerr D. Pharmacoadherence: an opportunity for digital health to inform the third dimension of pharmacotherapy for diabetes. J Diabetes Sci Technol 2021;15(1):177-183.
- Steenkamp D, Eby EL, Gulati N, Liao B. Adherence and persistence to insulin therapy in people with diabetes: impact of connected insulin pen delivery ecosystem. J Diabetes Sci Technol 2022;16(4):995-1002.
- Powers MA, Bardsley J, Cypress M, et al. DSMES in Adults With Type 2 Diabetes: A consensus report of the American Diabetes Association, the Association of Diabetes Care and Education Specialists, the Academy of Nutrition and Dietetics, the American Association of Family Physicians, the American Association of Physician Assistants, the American Association of Nurse Practitioners, and the Association of Pharmacists. The Science of Diabetes Self-Management Education and Care 2020;46(4):350-369
- Greenwood DA, Howell F, Scher L, et al. A framework for optimizing technology-enabled diabetes and cardiometabolic care and education: the role of the diabetes care and education specialist. Diabetes Educ 2020;46 (4):315-322.
- MacLeod J, Scher L, Greenwood D, et al. Technology disparities and therapeutic inertia- a call to action for the Diabetes Care and Education Specialist. ADCES In Practice. 2021;9(5):34-41| DOI: 10.1177/2633559X211032227.
- Friedman JG, Odugbesan O, Ebekozien O, Aleppo G; Increasing access to connected insulin pens by promoting shared decision-making through collaborative quality improvement. Clin Diabetes 15 October 2024; 42 (4): 470–473. https://doi.org/10.2337/cd24-0057
- Warshaw H, Isaacs D, MacLeod J. The reference guide to integrate smart insulin pens into data-driven diabetes care and education services. Diabetes Educ. 2020 Aug;46(4_suppl):3S-20S. doi: 10.1177/0145721720930183. PMID: 32779975.














-(1).png?sfvrsn=799e9a59_1)