Dr. Jeff Unger, MD, FAAFP, FACE
“If they have the risk of hypoglycemia, they will benefit from a CGM."
Dr. Unger feels that he can train a person on a CGM pretty quickly and that their glycemic control will start to improve within two weeks of initiation.
He directs his own primary care practice in Rancho Cucamonga, California. Dr. Unger operates a personal and professional CGM program and states that he doesn’t think he would be able to provide the best care to his patients who have diabetes without it.
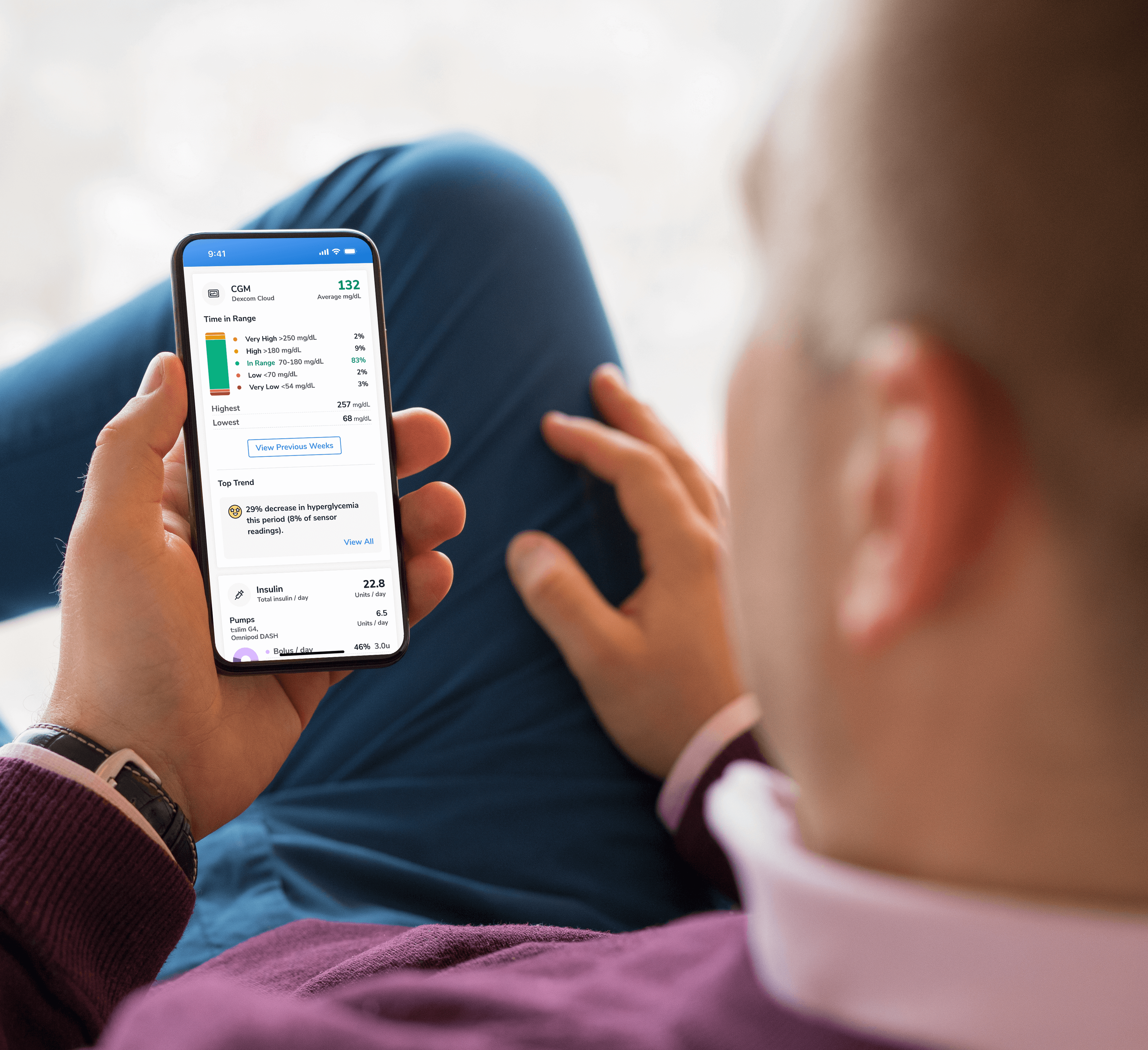
Most people with diabetes that he treats will receive a CGM, whether they have Type 1 or Type 2 diabetes. “If they have the risk of hypoglycemia, they will benefit from a CGM.” He states that health care providers benefit from their patients who have diabetes having a CGM by being able to see all the glucose data, 24 hours a day. This allows for being able to change treatment plans knowledgeably and safely. The people who have diabetes benefit from a CGM by being able to respond to trend arrows and often to avoid major glucose excursions. Dr. Unger feels that he can train a person on a CGM pretty quickly and that their glycemic control will start to improve within two weeks of initiation.
From his experience, people love the CGM and most people wear it 99% of the time. If a person with diabetes is thinking about going on an insulin pump soon, he takes that into consideration, and will help them choose a CGM that will integrate with the insulin pump that they are leaning toward. There are many choices of available CGM devices and Dr. Unger matches the patient’s need to the particular device.
Dr. Unger states that it is very important to do proper coding of the visit with the patient with diabetes. The diagnosis code for hypoglycemia is important to list, if applicable, and is a code that is sometimes overlooked. He takes an orderly approach to CGM interpretation and follows these steps:
1. Identify and correct hypoglycemia, aiming for a target of less than 4%.
2. Identify and correct post-prandial spikes in glucose.
3. Identify and correct glycemic variability, aiming for glucose time in range target of 70-180 mg/dl at least 70% of the time.
It takes him less than five minutes to complete the CGM interpretation and he will often compare it to the past office visit CGM data and use that as a teaching point to show the patient what sort of progress they have made.
Lastly, Dr. Unger strongly believes that it would be a disservice to the person with diabetes to not utilize personal CGM in the appropriate person. CGM gives you the benefit of being able to successfully treat your patients who have diabetes. CGM gives the provider a reason to praise the patient with diabetes, which Dr. Unger feels will help the patient do their best to remain adherent to their medication regimen. “Diabetes management is time-consuming and difficult for many patients.” CGM is a tool that can increase success with diabetes management and one that should be used much more often.
Dr. Anastasia Albanese-O’Neill, PhD, ARNP, CDCES
Every clinic that wants to initiate a personal CGM program needs a champion to get the program up and running and to continue to nurture and grow the program.
Dr. Anastasia Albanese-O’Neill, PhD, ARNP, CDCES, is the Director of Diabetes Education and Clinic Operations in the Division of Pediatric Endocrinology at the University of Florida in Gainesville. In 2015, UF Health pediatrics implemented a professional continuous glucose monitoring program. This gave patients the opportunity to experience a real-time CGM device and allowed the diabetes care team to review and interpret CGM data to inform patient care. In 2016, she launched the clinic’s personal RT-CGM training and education program. This structured program gave children served by the UF Health clinic the training and support required to use the RT-CGM device prescribed by their diabetes health care provider.
One of the first things that Dr. Albanese-O’Neill implemented was a “Wear and Share” program so that clinic staff and providers could wear the device. This gave them the opportunity to interact directly with the CGM, feel what it was like to insert it, experience alarms overnight, and set up the receiver and related Apps. This first-hand experience allowed providers, educators and staff to talk more confidently about the device with families.
A half day each week was designated for CGM training for people with diabetes and their family caregivers. Appointments were scheduled as a “CGM Start” with a nurse practitioner and Certified Diabetes Care and Education Specialist (CDCES). A suite of CGM-related resources were created in the electronic medical record (EPIC), including a Letter of Medical Necessity for CGM, a Referral to CGM clinic, and Assignment of Benefits form (so patient would know what the cost would be for the device and ongoing supplies). CGM documentation templates and visit summary templates with instructions were also created and available in EPIC. For the first year, devices were shipped directly to the clinic rather than the patient, due to problems in the past with patients forgetting to bring all components of the device or supplies with them to clinic on CGM start day.
During the training visit, comprehensive training for RT-CGM was provided. In addition, families were guided through setting up all related apps and linked to the clinic’s data sharing accounts. Written instructions were provided so families knew how to upload data to the clinic for review between clinic visits.
The workflow utilized a team approach for return visits. The clinic MAs checked the patient in, uploaded the patient’s device, and entered key variables into flowsheet in EPIC. The MAs also clipped the Ambulatory Glucose Profile and other glucose data into the visit template from Glooko or CLARITY. These data were readily available to clinicians during the visit to utilize for teaching, review with the family, and inform the diabetes care plan. The AGP was also pasted into the patient visit summary for goal setting.
An Advanced CGM course was offered that is cotaught by a nurse practitioner and CDCES. This class includes content on international guidelines for time in range (TIR), use of trend arrows, and factors impacting glucose levels. All clinic visit types had a written Standard Operating Procedure (SOP) that outlined the role of clinic staff and included a list of relevant EPIC templates, required referrals and related educational materials.
The billing process had been variable since program inception, but it has been revenue positive since 2018. The initial CGM placement for personal CGM was billed as CPT Code 95249. Review and interpretation of CGM data was billed with CPT Code 95251 following the placement and then at subsequent clinic visits when CGM data was interpreted during the clinic visit.
Ongoing resources for clinic staff included a weekly Diabetes Education and Clinic Operations meeting. The weekly meeting was attended by staff, fellows and providers and served as a forum to discuss metrics and opportunities to improve clinical outcomes using quality improvement principles.
Educational in-services were also provided during this scheduled weekly meeting. Dr. Albanese-O’Neill believes that every clinic that wants to initiate a personal CGM program needs a champion to get the program up and running and to continue to nurture and grow the program. She identifies challenges of personal CGM for the person with diabetes to be: initial cost, difficulty obtaining ongoing supplies, embarrassment with wearing a device, alarm fatigue, usability issues and data overload. She believes that these challenges can be overcome on an individualized basis and that the benefit of personal CGM outweighs the drawbacks.
Sara (Mandy) Reece, PharmD, CDCES, BC-ADM, BCACP, FADCES
When asked how she learned about CGM and prepared to add this to her practice, Mandy explained that the ADCES CGM Certificate Program was invaluable to her and this is where a lot of her knowledge came from.
Sara (Mandy) Reece, PharmD, CDCES, BC-ADM, BCACP, FADCES, is embedded within a family medicine clinic that is part of the Family Medicine Graduate Medical Education Program with Northeast Georgia Medical Center in Gainesville, GA, and she understands the value of offering both a professional and personal CGM program. Mandy performs team visits along with a physician or NP and is known as the “diabetes specialist” in her practice. She provides education for the other providers and residents about the CGM process; including how to interpret the Ambulatory Glucose Profile (AGP), how to prescribe CGM and understanding of the Medicare CGM requirements.
Her next goal is to develop a CGM training program for the practice’s support staff so they know about the ins and outs of CGM and will be able to identify people with diabetes who might benefit from CGM. Mandy began her CGM practice with professional CGM and now has integrated a personal CGM program into that. Both practices have been expanding rapidly. She also teaches personal CGM to eligible people with diabetes in the employee clinic. When asked how she learned about CGM and prepared to add this to her practice,
Mandy explained that the ADCES CGM Certificate Program (danatech. org) was invaluable to her and this is where a lot of her knowledge came from. She has encountered some barriers in obtaining personal CGM devices for all that would benefit from them. One barrier that she has come across is that the state Medicaid program does not cover CGM for people with Type 2 diabetes and has only limited coverage for people with Type 1 diabetes.
One way she has been able to still provide some CGM benefit for people without coverage for personal CGM is through offering professional CGM. As a pharmacist, Mandy brings many important skills to the CGM process in her practice. She assists the person with diabetes with device selection, checks insurance benefits, directs person where to go to obtain their CGM, provides training about the CGM, provides individualized CGM settings, troubleshoots any problems that the person is experiencing related to their CGM and downloads and interprets data. Mandy advises to be cautious with setting CGM alerts in the beginning of device wear. This will minimize early frustrations due to alarms. These alerts can be adjusted as you go along. She also states the importance of starting a CGM with realistic expectations.
Mandy tells people who are new to CGM that “it is a tool to help you better understand your diabetes, not a cure all.” Common concerns that she addresses with people who have been using their CGM for a while include the device getting knocked off their arm, sweating too much and it falls off and worries about the fingerstick blood glucose value and the CGM interstitial glucose value not matching up.
Mandy shares two recommendations related to CGM:
1. Sign up for the ADCES Putting CGM into Practice: Certificate Program (2nd Edition)
2. Look for practice opportunities for both personal and professional CGM. CGM will help make the picture clear as to why someone’s diabetes is not well managed. Her advice to practices that have not started a CGM program yet is that if you are measured by quality measures, CGM will improve your quality metrics. Secondly, CGM will empower your patients and increase their satisfaction with you as their provider. It truly is a win-win.














-(1).png?sfvrsn=799e9a59_1)